-
What are Achilles Tendon Injuries
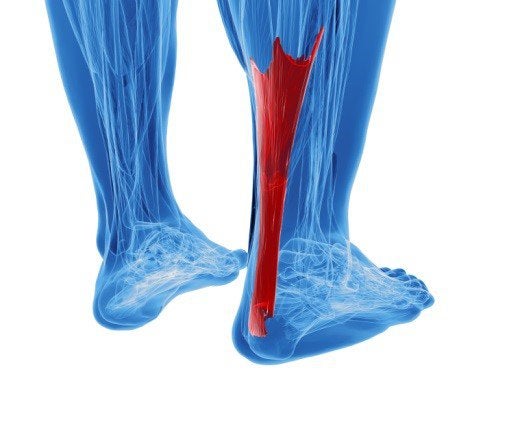
The Achilles tendon is the strongest tendon in the human body. Its purpose is to connect the lower leg muscles and calf to the heel of the foot. This tendon is responsible for facilitating all types of movement, like walking and running. This tendon provides an enormous amount of mobility for the body. Any injuries inflicted to this tissue should be immediately brought up with a physician to prevent further damage.
The most common injuries that can trouble the Achilles tendon are tendon ruptures and Achilles tendinitis. Achilles tendinitis is the milder of the two injuries. It can be recognized by the following symptoms: inflammation, dull to severe pain, an increased flow of blood to the tendon, thickening of the tendon, and slower movement time. Tendinitis can be treated via several methods and is often diagnosed by an MRI.
An Achilles tendon rupture is trickier to heal, and is by far the most painful injury. It is caused by the tendon ripping or completely snapping. The results are immediate and absolutely devastating, and will render the patient immobile. If a rupture or tear occurs, operative and non-operative methods are available. Once the treatment begins, depending on the severity of the injury, recovery time for these types of issues can take up to a year.
Simple preventative measures can be taken as a means to avoid both injuries. Prior to any movement, taking a few minutes to stretch out the tendon is a great way to stimulate the tissue. Calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses are all suggested ways to help strengthen the lower legs and promote Achilles tendon health.
Many problems arise among athletes and people who overexert themselves while exercising. Problems can also happen among those who do not properly warm up before beginning an activity. Proper, comfortable shoes that fit correctly can also decrease tendon injuries. Some professionals also suggest that when exercising, you should make sure that the floor you are on is cushioned or has a mat. This will relieve pressure on the heels. A healthy diet will also increase tendon health.
It is very important to seek out a podiatrist if you believe you have an injury in the Achilles region. Further damage could result in severe complications that would make being mobile difficult, if not impossible.
-
Achilles Tendonitis One of Many Foot and Ankle Injuries
 Known as the thick tendon that connects your calf muscles to your heel bone, the Achilles tendon allows you to do everyday activities such as walking and running. Insertional Achilles tendonitis is a condition of the Achilles tendon in which pain is experienced at the heel, and which can become chronic if left untreated. Non-insertional Achilles tendonitis can be described as a microscopic tearing of the fibers in the tendon. If the problem becomes chronic, a bone spur can eventually develop as the tendon thickens. If severe, the condition may require surgery.
Known as the thick tendon that connects your calf muscles to your heel bone, the Achilles tendon allows you to do everyday activities such as walking and running. Insertional Achilles tendonitis is a condition of the Achilles tendon in which pain is experienced at the heel, and which can become chronic if left untreated. Non-insertional Achilles tendonitis can be described as a microscopic tearing of the fibers in the tendon. If the problem becomes chronic, a bone spur can eventually develop as the tendon thickens. If severe, the condition may require surgery. Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Dr. Jon M. Sherman of Kentlands Foot & Ankle Center . Our doctor will assist you with all of your foot and ankle needs.
What is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can cause severe difficulties and should immediately be presented to a doctor.
What are the symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
– Inflammation
– Dull to Severe Pain
– Increased blood flow to the tendon
– Thickening of the tendon
Rupture Symptoms
– Extreme pain and swelling in the foot
– Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
– Thorough stretching of the tendon before and after exercise
– Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our office located in Gaithersburg, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Read more about Achilles tendon injuries.
-
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
-
How to Tell If You Have Plantar Fasciitis
 If you’re experiencing stiffness and pain in the soles of your feet that typically becomes more prominent during the mornings, you may have plantar fasciitis . Plantar fasciitis can be described as a foot condition that results from overuse of the plantar fascia, the tissue that runs along the soles of your feet. Excessive stress on this area can lead to inflammation. Being overweight, having flat feet or high arches, pregnancy and improper footwear such as flip flops are also factors in the development of plantar fasciitis. Treat your condition by icing your feet, stretching your muscles and having proper rest by avoiding any strenuous activity.
If you’re experiencing stiffness and pain in the soles of your feet that typically becomes more prominent during the mornings, you may have plantar fasciitis . Plantar fasciitis can be described as a foot condition that results from overuse of the plantar fascia, the tissue that runs along the soles of your feet. Excessive stress on this area can lead to inflammation. Being overweight, having flat feet or high arches, pregnancy and improper footwear such as flip flops are also factors in the development of plantar fasciitis. Treat your condition by icing your feet, stretching your muscles and having proper rest by avoiding any strenuous activity. Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Jon M. Sherman of Kentlands Foot & Ankle Center . Our doctor will assist you with all of your foot and ankle needs.
What is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
· Excessive running
· Non-supportive shoes
· Overpronation
· Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
· Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
· Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
· Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in Gaithersburg, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Read more about Plantar Fasciitis
-
Systemic Diseases of the Foot
There are several systemic diseases, or diseases that affect the whole body, that either display symptoms in the feet or affect the health of the feet. Common systemic diseases that affect the overall health of the feet, and the patient’s ability to walk comfortably, include gout, diabetes mellitus, neurological disorders, and arthritis.In gout, which is caused by an excessive buildup of uric acid in the body, the most common symptoms of pain, inflammation, and redness occur at the metatarsal/phalangeal joint at the base of the big toe. Any excess levels of uric acid, crystallize and are deposited in tendons, joints, and surrounding bone and muscle tissue. Gout is commonly treated with NSAIDs to relieve pain and inflammation and other drugs to lower uric acid levels in the body. Gout most commonly affects those who are overweight, have low protein diets and lead a more sedentary lifestyle.
Diabetes mellitus is an increase in the level of blood sugar in which the body cannot counteract with naturally occurring insulin in the body. The three types of diabetes, Type I, Type II and Gestational Diabetes, are all signs the body is either not producing enough insulin or is not efficiently using the insulin that is produced. Gestational diabetes only affects women who are pregnant and have never, prior to pregnancy, exhibited symptoms of the disease.
There are two main issues that affect the feet that are commonly caused by diabetes. They include diabetic neuropathy and peripheral vascular disease. Diabetic neuropathy can lead to damaged nerves and affect the feet through numbness and loss of sensation. Peripheral vascular disease restricts the flow of blood to the foot and can, in extreme cases, lead to the necessity of amputating the foot. Peripheral issues that are caused by diabetes and can affect the foot include athlete’s foot, nail infections, corns, blisters, bunions, severe dry skin, plantar warts and ingrown toenails. These can all be attributed to the decrease of blood flow to the foot.
Neurological disorders and rheumatoid arthritis can also have severe impact on the health of the feet. Neurological disorders can affect the nerves in the main structure of the foot and cause loss of sensation and possible decreased muscle response. Rheumatoid arthritis can affect the bones and joint structures of the foot, making it impossible to walk normally without serious pain.
All systemic diseases that affect the foot can effectively be treated to minimize joint and muscle damage if they are diagnosed early and treated with medication and lifestyle therapy. Diabetes patients must monitor their blood sugar levels and work with their physician to keep their levels as close to normal as possible. Rheumatoid arthritis patients should work with their physician to ensure the proper medications are being taken to reduce the amount of damage to the joints of the body.
-
Burning Sensation in the Feet
 If you have symptoms of a burning sensation in your feet , you may have any number of conditions. The sensation of burning in the feet can be either minor or severe, affect people over 50, and occur most frequently during the night. Nerve damage from diabetes, vitamin deficiency or alcoholism, obesity, strain on the feet, overheated feet, eczema or dermatitis, blood disorders, or any other impairment of the feet’s nerves can all lead to the described burning sensation. Seeing your podiatrist is vital to understanding any underlying causes. Make sure that you are wearing properly-fitting shoes as well.
If you have symptoms of a burning sensation in your feet , you may have any number of conditions. The sensation of burning in the feet can be either minor or severe, affect people over 50, and occur most frequently during the night. Nerve damage from diabetes, vitamin deficiency or alcoholism, obesity, strain on the feet, overheated feet, eczema or dermatitis, blood disorders, or any other impairment of the feet’s nerves can all lead to the described burning sensation. Seeing your podiatrist is vital to understanding any underlying causes. Make sure that you are wearing properly-fitting shoes as well. When dealing with systemic disease of the feet, is extremely important to check the affected areas routinely so that any additional problems are caught quickly. If you have any concerns about your feet and ankles contact Dr. Jon M. Sherman of Kentlands Foot & Ankle Center . Our doctor will assist you with all of your foot and ankle needs.
Systemic Diseases of the Feet
Systemic diseases affect the whole body, and symptoms usually are displayed in the feet. This condition can make a patient’s ability to walk unbearable. Systemic diseases include gout, diabetes mellitus, neurological disorders, and arthritis.
Gout – is caused by an excess of uric acid in the body. Common symptoms include pain, inflammation, and redness at the metatarsal/phalangeal joint of the base big toe. Gout can be treated by NSAIDs to relieve pain and inflammation, and other drugs that lower the acid levels in the body.
Diabetes mellitus – is an increase in the level of blood sugar that the body cannot counteract with its own insulin. Failure to produce enough insulin is a factor in Diabetes.
Diabetes of the Feet
Diabetic Neuropathy – may lead to damaged nerves and affect the feet through numbness and loss of sensation.
Peripheral Vascular Disease – can restrict the blood flow to the feet, and often times lead to amputation of the feet.
If you have any questions please feel free to contact our office located in Gaithersburg, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Read more about Systemic Diseases of the Feet
-
Arthritic Foot Care
During your lifetime, you will probably walk about 75,000 miles, which is quite a lot of stress to put on your feet. As you get older, the 26 bones and 30 joints in each of your feet will lose flexibility and elasticity. Your foot’s natural shock absorbers will wear down as well. Having arthritis added to this mix only makes matters worse. Your joints will become distorted and inflamed, which is why arthritic foot care needs to be something to think about every day.
When dealing with arthritis, having additional foot complications, such as bunions, hammertoes, or neuroma, can be a serious detriment. To avoid these, buy well-fitting shoes with a lower heel and good support. Arthritis causes you to lose your arch, so having shoes with good arch support is also highly recommended.
Aside from getting good arch support, the shoes need to fit comfortably and properly as well. A good place to start is by leaving a finger width between the back of the shoe and your foot to gauge proper size. It is also helpful to have a square or rounded toe box in the front to provide even more comfort. Another thing to look for is a rubber sole that can provide a cushion and absorb shock as you walk. This adds flexibility to the ball of your foot when you push off your heel to walk.
Exercise is another key aspect of arthritic foot care. Exercise not only strengthens and stretches your muscles and joints, but helps to prevent further injury and pain as well. Stretching the Achilles tendon, the tendon located in the back of your heel, will give you added mobility and reduce pain due to stress. Another thing you can do is massage your feet, kneading the ball of your foot as well as your toes from top to bottom.
Stretching the Achilles tendon is a simple exercise that you can do at home anytime. Lean against the wall with your palms flat against the surface while placing one foot forward, towards the wall, and one foot behind you. Bend your forward knee towards the wall while keeping your back knee locked straight, and make sure both your heels are completely touching the ground at all times. This will stretch your Achilles tendon and calf muscles as well. You will feel the stretch almost immediately. You can also stretch your toes in a couple ways. One involves taking a rubber band and wrapping it around both your big toes while your heels remain together. Then, pull them apart to stretch your big toe. You can also place a rubber band around all the toes of one of your feet. Then, try to separate each individual toe, stretching them all.
A final step you can take to help your arthritis is taking non-steroid, non-inflammatory drugs or topical medicines with capsaicin. Unfortunately, there is no complete way to remove all of your arthritic pain. However, following some of this advice can go a long way in staying as pain-free as possible.
-
CDC Releases Report on Arthritis
 Arthritis is a condition that affects not only the hands and wrists, but feet and ankles as well. There are more than 50 million people in the US that are currently diagnosed with arthritis and there are a lot of different opinions on how to effectively treat the disease. Frequently it is difficult to parse through what does work and what doesn’t. Arthritis can be painful, especially when it affects the foot and ankle area. When trying to manage this pain, it is important to be informed on what types of treatments are effective, keeping in mind that some can actually be harmful. The CDC has recently released a report that outlines some good and bad treatments for this chronic ailment.
Arthritis is a condition that affects not only the hands and wrists, but feet and ankles as well. There are more than 50 million people in the US that are currently diagnosed with arthritis and there are a lot of different opinions on how to effectively treat the disease. Frequently it is difficult to parse through what does work and what doesn’t. Arthritis can be painful, especially when it affects the foot and ankle area. When trying to manage this pain, it is important to be informed on what types of treatments are effective, keeping in mind that some can actually be harmful. The CDC has recently released a report that outlines some good and bad treatments for this chronic ailment. Arthritis can be a difficult condition to live with. If you are seeking treatment, contact Dr. Jon M. Sherman of Kentlands Foot & Ankle Center . Our doctor will assist you with all of your foot and ankle needs.
Arthritic Foot Care
Arthritis is a joint disorder that involves inflammation of different joints in your body, such as in your feet. Arthritis is often caused by a degenerative joint disease and causes mild to severe pain in all affected areas. On top of this, swelling and stiffness in the affected joints can also be a common symptom of arthritis.
In many cases, wearing ill-fitting shoes can worsen the effects and pain of arthritis. Wearing shoes that have a lower heel and extra room can help your feet feel more comfortable. In cases of rheumatoid arthritis, the arch in your foot may become problematic. Buying shoes with proper arch support that contour to your feet can help immensely.
Alleviating Arthritic Pain
- Exercises that stretch the foot can prevent further pain and injury and increase mobility
- Most of the pain can be alleviated with anti-inflammatory drugs, heat, and topical medications
- Massages can help to temporarily alleviate pain.
It is best to see your doctor for the treatment that is right for your needs and symptoms. Conditions vary, and a podiatrist can help you determine the right method of care for your feet.
If you have any questions please feel free to contact our office located in Gaithersburg, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Read more about arthritic foot care
-
Stress Fractures more Common for Athletes in Team Sports
 The fifth metatarsal is the long bone that connects to the pinky toe on the outside of the foot. This bone is especially prone to fracture for people involved in any sort of prolonged physical activity, especially team sports. A stress fracture is one of the most common injuries in soccer, but many other athletes also suffer this injury. It is vitally important to never ignore any type of foot pain, on the field or off. Professionally, there is immense pressure to perform, which can lead to dependency on prescription painkillers. But the truth is, we all need our feet, not just star athletes. The best course of action is always to contact a podiatrist and get to the root of the problem.
The fifth metatarsal is the long bone that connects to the pinky toe on the outside of the foot. This bone is especially prone to fracture for people involved in any sort of prolonged physical activity, especially team sports. A stress fracture is one of the most common injuries in soccer, but many other athletes also suffer this injury. It is vitally important to never ignore any type of foot pain, on the field or off. Professionally, there is immense pressure to perform, which can lead to dependency on prescription painkillers. But the truth is, we all need our feet, not just star athletes. The best course of action is always to contact a podiatrist and get to the root of the problem. Activities in which too much pressure is placed on the feet can cause stress fractures. If you have any concerns about your feet contact Dr. Jon M. Sherman of Kentlands Foot & Ankle Center . Our doctor will treat your foot and ankle needs.
Dealing with Stress Fractures of the Foot and Ankle
The Stress Fractures occur on the foot and ankle when muscles in these areas weaken from too much or too little use. Then the feet and ankles lose support when walking or running from the impact of the ground. Since there is no protection the bones receive the full impact of each step. The stress on the feet causes cracks to form in the bones, thus called stress fractures.
What are Stress Fractures?
Stress fractures occur frequently in individuals whose daily activities cause great impact on the feet and ankles. Stress factors are most common among:
- Runners
- People affected with Osteoporosis
- Play tennis or basketball
- Gymnastics
- High impact workouts
Symptoms
Pain from the fractures occur in the area of the fractures, and can be constant or intermittent. It will often cause sharp or dull pain with swelling and tenderness. Engaging in any kind of activity that involves in high impact will aggravate pain.
If you have any questions please feel free to contact our office located in Gaithersburg, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Read more about Stress Fractures of the Foot and Ankle
-
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures are small breaks in the bone that are caused by repetitive stress. They typically occur due to overuse, forcing the bones of the foot or ankle to continually absorb the full impact of each step someone takes. Stress fractures can also be caused by abnormal foot structure, osteoporosis, bone deformities, or wearing improper footwear during exercise.
Stress fractures are common for individuals whose daily activities cause high levels of impact on their feet and ankles. Individuals who run, play tennis or basketball, or practice gymnastics tend to experience these fractures more frequently. Anyone is susceptible to this problem, though. Individuals who are normally sedentary and suddenly begin an intense, high impact workout may sustain stress fractures. This is because their muscles are not yet strong enough to handle and cushion the intensity of their activity. Osteoporosis may also cause someone to get stress fractures, because the disease weakens an afflicted person’s bones and makes it easier for them to break down.
Pain from stress fractures typically occurs in the general area of the fracture. Pain can also manifest as “pinpoint pain” or pain that is felt when the site of the injury is touched, and can be accompanied by swelling. It may occur during or after activity, and it may disappear while resting and return when standing or moving. Engaging in any kind of activity, high impact or otherwise, will aggravate the pain. If the intensity of the activity increases before the stress fracture has properly healed, it can cause a full fracture.
Treatment can vary depending on the individual and the degree of injury. The primary way to treat a stress fracture is to rest the hurt foot. Some fractures will heal quickly with only a little bit of rest, while others may require a long rest period and the use of crutches, immobilization, or physical therapy. Under certain circumstances, surgery may be required to install support pins around the fracture to assist in healing.
If you are undergoing a new exercise regimen in running or some other kind of high impact activity, set incremental goals on a weekly basis so you can build up muscle strength. Make sure to wear supportive shoes to better protect you feet.
If you begin to experience any symptoms of stress fractures, you should stop exercising and rest. If the symptoms persist, consult with your podiatrist. Remembering these tips can help you prevent stress fractures to your foot and ankle, and allow you to continue living normally.
RECENT POSTS
categories
- Uncategorized
- Featured Articles
- Foot Disorders
- Broken Ankle
- Broken Toe
- Fracture
- Foot Health
- Foot Care
- Arthritis
- Foot Pain
- Skin Cancer
- Podiatry Appointment
- Custom Orthotics
- Podiatrist
- Diabetes
- Gout
- Heart Health
- National Nutrition Month
- National Foot Health Awareness Month
- Foot Safety
- Foot and Ankle Injuries
- Falls Prevention
- Chronic Heel Pain
- Shoes
- Laser Therapy
- Quoted
- Physical Therapy
- KeryFlex
- Sweat
- Summer Foot Care
- Sports Injury
- ESWT
- Fungal Toenails
- Bunion


